Sore calves are no joke – especially if you’ve ever experienced jolting awake in pain at night. If sore calves have you worried, then stop. The phenomenon is actually very common. About 60% of adults experience nocturnal calf pain or cramps, according to studies.
Recurrent painful calf cramps can be so severe at times, they may prevent you from sleeping – resulting in insomnia and significantly impacting your life in more ways than one. At [Injurymap](https://www.injurymap.com/], we understand how serious this condition can be and want to help you deal with sore calves through this informative guide.
Calf Muscles: Basic Anatomy
Our legs bear the brunt of most of our actions, absorbing impact forces from the ground and transmitting body forces against gravity. Continued pain and soreness can become a major worry, as it impacts your whole life. Before listing reasons for your calf soreness, here are a few details you must know about the anatomy of the calf.
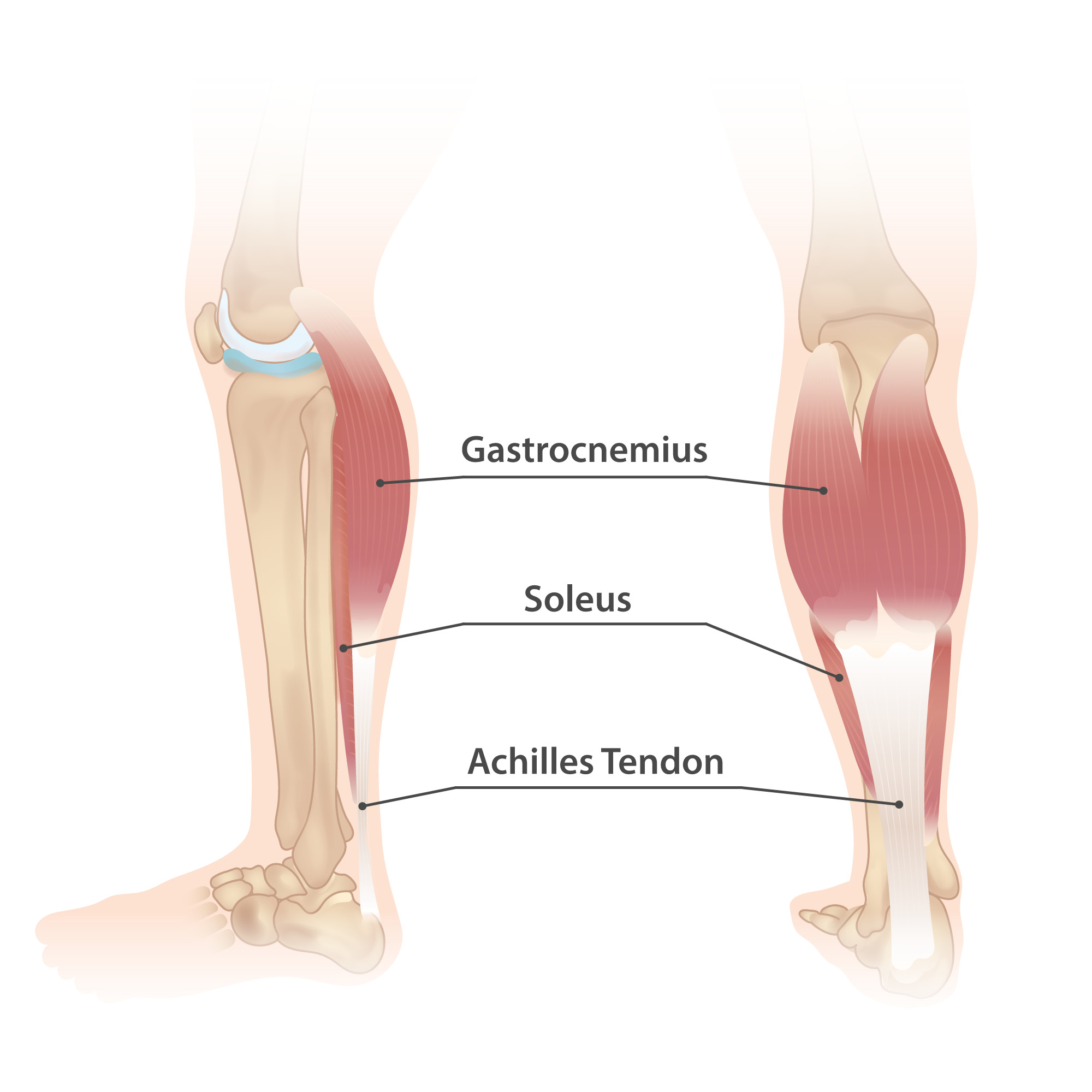
The calf forms the back part (or “posterior compartment”) of the leg. Two muscles make up the bulk of the calf. These are the larger gastrocnemius and the smaller soleus muscle. The gastrocnemius muscle is the superficial, bulging muscle visible to us all. Its two heads give it a distinct diamond shape – like we can see in athletes and military personnel.
The soleus lies under the gastrocnemius and is flat. Together they merge and taper to the base of the heel. There they are interlinked by connective tissue and attach to the Achilles tendon. The tendon itself is inserted into the calcaneus bone of the heel.
Throughout the calf muscles is a network of veins, arteries and nerves. The calf muscles and the deep veins have a network of valves and pumps. This system is called your “peripheral heart.” This is because, when you’re in an upright position, the calf muscles work against gravity to close the valves – contracting and driving blood from your legs towards your heart.
When the calf muscles relax, it allows the valves to open and the veins fill with blood. With each contraction, this “peripheral heart” drives about 40 – 60% of the blood towards your heart.
Your calf muscles are themselves supplied by the popliteal artery. This is a branch of the femoral artery, the main artery of the leg that comes from the aorta. The popliteal artery then splits further into anterior and posterior tibial arteries supplying oxygen and nutrients to the ankle, foot, heel, and sole.

As far as the nervous supply is concerned, the major nerve of the leg is the sciatic nerve which starts in the lower back and reaches the lower leg through various branches like the peroneal nerve, tibial nerve and saphenous nerve, as illustrated below.

Common Reasons Your Calves Feel Sore
Keeping in mind the basic anatomy of the calf muscles, we can now look at some of the common reasons you may experience sore calves or lower leg pain. While the way the pain appears may differ, you might find that all of them tend to have very similar symptoms. Cramps, inability to move the leg, swelling, and pain.
DOMS
Delayed Onset Muscle Soreness or DOMS is the pain and soreness individuals experience after a strenuous workout. It usually appears almost 24 to 72 hours after exercise. This usually occurs if you’ve just begun or restarted exercising after a long period of inactivity. It can also happen if you overexert your muscles. Because it can appear almost two days after your workout it is called delayed onset muscle soreness and is often confused for a muscle tear.
What does DOMS feel like? Your calf muscle will feel cramped. It will feel weak and the pain may be a dull throb that doesn’t go away. Dehydration can worsen DOMS. Keeping up hydration can therefore help. However, as you exercise and the muscles adapt to the added stress, it will decrease with time.
Calf Muscle Strain
Calf muscle strains involving the soleus and gastrocnemius muscles usually occur when the two have been overstretched during exercise. These muscles are located in the back of your leg and make up the bulk of your calf. The muscle fibers have some degree of tears which result in muscle inflammation and pain. You will find the pain right in the middle of the belly of the calf. Most calf strains occur due to forceful uncoordinated motion or during high motion events, like running or cycling. Muscle strains are usually graded.

Grade 1: This is a mild tear of a few muscle fibers. Here you’ll find the muscle is painful on touch but maintains its normal strength. You can walk and use your legs without your range of motion being affected.
Grade 2: This grade involves a higher percentage of tears in the muscle fibers but not a complete tear. During the injury, a few of your muscle fibers may snap which makes the muscle extremely painful. Since it’s not a complete tear, symptoms may appear gradually. There may be a visible loss of strength and movement is affected. Often, the individual may limp and the range of motion is decreased.
Grade 3: This is a severe tearing of the muscle fibers. It could also be a complete muscle tear where the entire muscle is torn. The muscle may “pop” when the injury occurs. Obvious bruising occurs, and you can see the tear as a dent. The leg has to be rested as movement is excruciating. Weight bearing on your leg is out of the question. You have to see a doctor for this condition.
Muscle Cramps
Muscle cramps are sudden and appear out of nowhere. They can happen while you’re lying down or walking around. They can make your calf muscles feel very hard and tight. The sensation of “pins and needles” best sums up how you may feel during cramps. They are short-lived and should resolve within minutes. You can simply elevate the leg and wait till it passes away.
Contusion
Any injury or direct blow to the calf muscle will not only tear the muscle fibers but also break the blood vessels supplying them. This causes the blood to ooze out of the vessels into the surrounding tissue – leading to muscle swelling and pain. A bruise develops as the blood spills over. Bruising is visible under the skin. If it continues to grow it may develop into a hematoma.
Tendinitis
Calf pain is one of the first signs something is wrong with your Achilles tendon. Since your calf muscles are connected to this tendon, they are the first to feel it, if there’s a tear or rupture of your Achilles. A tendon rupture may feel like a sudden pop in the leg.
In elderly individuals, standing up or walking can cause it to rupture, especially if it has been weakened by a previous tear. In younger people and athletes, forced, abrupt movement can cause the tendon to tear and become inflamed. Ice the area and raise your foot. Do not bear any weight on the affected leg. If you hear or feel a pop, visit your doctor immediately.
Deep Vein thrombosis
Deep Vein thrombosis or DVT occurs when your veins develop blood clots. These usually start in the legs. The blood clots can be dangerous as they can travel towards the lungs and cause a pulmonary embolism. When they start in your legs, the calf muscles develop cramps.
Your calves may swell, and feel warm and tender to the touch, and your skin may appear red. If you see these symptoms, visit the emergency room immediately. This is one condition you want to get checked right now.
Peripheral artery disease
Peripheral artery disease or PAD occurs when the circulating blood vessels are affected due to narrowing of the arteries. It can be precipitated by smoking and deposition of fat in your arteries. As the arteries narrow, the blood supply to the legs is reduced. The muscles are starved of oxygen and nutrients.

Along with having a sore calf, you may find areas of the leg will be cold or numb. If you find your leg is turning cold, see a doctor right away. The longer the leg remains without blood the more dangerous it is.
Often the pain worsens on walking or during movement, when the demand for oxygen increases. The skin on the leg may become very shiny and pale. Sometimes, the toenails become brittle. If it worsens, sores may appear on your legs which can take a long time to heal.
Lumbar Canal Stenosis
The lumbar vertebrae consist of five spinal bones. If your spinal column narrows, the nerve roots, and the spinal cord in this area are affected, producing symptoms in the sciatic nerve running down the leg. Stenosis or the narrowing of spaces in your spinal column is a degenerative process in those over sixty.
Over decades, the intervertebral discs lose height as they become less flexible and bony spurs may grow into the foramina, narrowing the space.
Stenosis or the narrowing of spaces in your spinal column is a degenerative process in those over sixty. Pain may radiate down your legs and calves. Your calves may cramp on walking and require frequent rest to relieve the pain. The pain may improve on lying down or sitting.
Cirrhosis
Muscle cramps usually occur in liver disease. How they occur remains unclear. Studies have shown that people suffering from chronic cirrhosis tend to develop muscle cramps that are intermittent and not constant as in varicose veins.
They also have other symptoms like bloated abdomen, difficulty breathing, liver spots on the skin, spider veins around the navel and elevated blood pressure in the portal vein. 70% of cirrhosis sufferers develop these cramps in their calves. Your cramps may be intermittent, yet severe enough to affect your quality of life and movement.
Varicose Veins
These large twisted, purple veins occur when the valves and pumps in your venous network weaken and fail to work properly. As a result, when the calf muscles contract, the valves fail to close and pump the blood back to the heart. Blood starts pooling in the veins, leading to their spidery, bulging and tortuous appearance.
Apart from this, you may feel a deep ache within the calf muscle. The pain might be a burning or throbbing and you may also experience some itchiness around the veins. If you’re in a job where you find yourself standing all day, then try to take sitting breaks. Or start wearing compression stockings to help your veins.
Neuropathy
Neuropathic pain usually occurs when the nerves are affected by diabetes, infections, nerve conditions and other metabolic problems. This pain can result in weakness and numbness of the calf muscles if the nerves of the leg are involved.
Sometimes the pain can be worse at night. So bad that it can be disabling, which is why you need to monitor your sugar levels and have your infections treated by the right antibiotics.
Restless Leg Syndrome
Restless leg syndrome is also called Willis-Ekbom Disease. It’s more of an unpleasant sensation where you may experience an irresistible urge to move your legs – hence the name “restless leg” syndrome. The sensation worsens at night and can cause insomnia. People have to get out of bed and walk around to get rid of the cramps. The cause for this is unknown.
Red Flags: What To Look Out For And When To See A Doctor
While calf pain is always secondary to some other underlying disease, it’s important to be aware of the red flags. Certain complications of calf pain can be life threatening and will require immediate treatment. We’ll show you how to spot them and have them checked by a medical professional at the earliest. Some of them can turn into medical emergencies and can be fatal if left unchecked.
- Hematomas: If you can see a hematoma growing following a calf contusion injury, then you need to see a doctor. Usually, the body seals off broken blood vessels through its clotting process. If however, your body is failing to do so, it’s because the injury is too severe. Since the compartments in the leg have limited space, large pools of blood can add pressure to the muscles and cause compartment syndrome.
- Inability to walk: Achilles tendon ruptures, even partial ones, can impair movement. If you find that you can’t walk or walking produces too much pain, then you need to seek help. Respiratory Distress: One of the signs that DVT has sent a blood clot to your lungs is difficulty in breathing. If you have sudden shortness of breath, chest pain, dizziness or you suddenly start coughing up blood, rush to an emergency room.
- Change in Sensation: If you lose sensation, or your feet turn cold, then there’s a chance that the arterial supply and nervous supply are compromised. To restore them immediately it’s best to have them checked out at the earliest.
- Joint Effusion: Joint swellings of any kind that cause calf pain have to be examined carefully. If you have swollen joints, then they must be seen by a specialist.
- Ulcers: Any ulcers or open sores along the calf and leg must be investigated further. If they’re not healing, then they must be examined. Sores reflects a failure of the body to self-heal.
- Compartment Syndrome: If your leg appears comparably red and tight, with the pain escalating, you might be developing compartment syndrome. This must be seen by a doctor who will try and relieve the pressure between the muscles.
- 6P’s: If you’re experiencing the 6 P’s— Pain, Pallor, Paralysis, Paresthesia (abnormal sensation), Pulselessness and Poikilothermia (abnormal temperature), see a doctor now!
Diagnosing Calf Soreness
A doctor will ask you to describe your symptoms in detail. You might find the questions too intrusive, but the quality of pain, frequency, time of day, all matter as it will help pinpoint the cause of your pain.
In addition, they will perform a very thorough medical examination. For example, Homan’s test which is compressing the calf is done to confirm DVT or the straight leg test is done to check for sciatica. These initial tests help you get started on preliminary treatment. The physical examination helps the doctor identify the primary cause of your calf pain. Is it the muscle, the tendon, vein, artery or nerve that is the source of your calf pain?
Doctors make you perform a series of maneuvers like Thompson test and Garrick test where the doctor will ask you to raise your leg, flex and plant your feet. It may all feel unnecessary but these tests help narrow down which muscle, which nerve and blood vessel is responsible for your pain. The Homan’s test is indicative of a venous issue while the straight leg test, pinpoints a nerve problem.
Doctors may suggest doing a Doppler Ultrasound to visualize your veins. A normal ultrasound can produce images but cannot monitor your blood flow. A Doppler ultrasound differs from a normal ultrasound because it can show the blood flowing through your veins or if there is any obstruction.
Your doctor may ask for X-rays to see your tendons and joints. They may also request for CT’s (Computerized Tomography scans) or MRI’s (Magnetic Resonance Imaging) if they want to look at the joints and the spinal column. In addition, they may perform nerve conduction studies. These are studies where the doctors measure how fast the electrical impulses are being sent across your nerve.
They may even ask for blood samples to check you for diabetes, liver function, and metabolic syndrome. If they suspect a blood clot, they may ask for D dimer tests. D dimer is protein fragment of blood clots. It’s very specifically used to check if you have DVT. For arterial conditions, they may ask for an angiography. This is like an Xray, done by introducing a dye into your blood stream. It’s specifically used to see the blockages of your arteries.
Be prepared to give a list of the medications you take. Drugs like iron sucrose, conjugated estrogens, raloxifene, naproxen, and teriparatide are strongly associated with nocturnal leg cramps..
Treat Calf Pain
The treatment of calf pain depends entirely on the cause.
- Rest: The first thing you must do when you have calf pain is decrease of activity, or rest. You’re overexerting the muscles that are already partially torn and need time to recover. Very often this is the only step required to relieve any calf soreness and pain following intense exercise.
- Elevate: Raise your leg so gravity won’t work against your veins and muscles. By elevating your leg, you put less pressure on the valves and pumps in the venous system to send blood back to the heart.
- Ice and Heat: Depending on the cause of your pain, applying ice packs or heating pads will help.
- Compression Stockings: If you have varicose veins doctors may suggest wearing compression stockings to aid the calf muscles.
- Medications: Medications to help thin the blood and relieve the pain may be prescribed to you depending on the cause of the pain.
- Surgery: If you have a tendon or a muscle rupture, you will require surgery.
- Massages: The jury is still out on whether massages really help relieve calf pain but athletes swear by it and so you can try using a foam roller to relieve some muscle tension.
- Physical therapy: This is by far the best way to treat calf pain. It forms part of every therapy, irrespective of the cause. Here we provide an extensive list of stretches and progressive strengthening exercises, so that you’re not fighting calf pain daily.